We can use stem cells to make embryos. How far should we go?
This article is from The Checkup, MIT Technology Review’s weekly biotech newsletter. To receive it in your inbox every Thursday, sign up here.
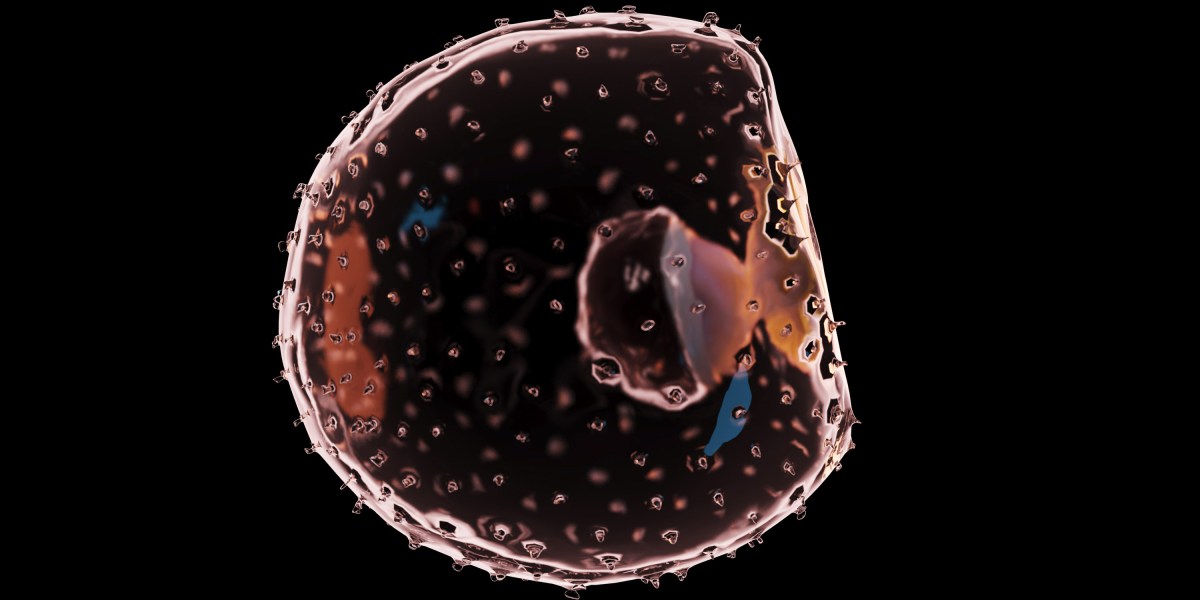
Embryos are special. These tiny blobs of cells have the potential to create life. That’s why we limit what scientists can do with them. Researchers are generally not allowed to grow human embryos for more than 14 days, for example.
But what about embryo-like structures made from stem cells? These “synthetic embryos” can be made without the direct contribution of egg or sperm cells. Because they’re not “real” embryos, some have argued that the same restrictions don’t apply.
Recent advances are allowing scientists to create embryo-like structures that look more and more like the real thing. Just this week, scientists in China described how they developed structures called blastoids for 17 days in the lab. They even managed to get some of them to implant in the uteruses of monkeys and trigger the very first signs of pregnancy.
The blastoids didn’t survive for very long, probably because researchers haven’t quite figured out how best to mimic what happens during the development of a conventional embryo. But most believe that it’s just a matter of time. If we can eventually get stem cells to form a viable embryo, a functional fetus, or even a baby, should we treat blastoids in the same way we treat embryos?
First, a bit more on the rule that human embryos should not be grown in labs beyond 14 days after fertilization, which was recommended by a UK government committee back in 1984. Since then, it has been enshrined in law in at least 12 countries, including the US.
Why 14 days? One reason is that this is just before an embryo develops three layers of cells that eventually go on to form its organs and tissues. Another is that this is around the time when the embryo is no longer able to split and form twins, so it is set on course to become an individual.
Today, most scientists believe that the cutoff is a pretty arbitrary one. When I asked Susana Chuva de Sousa Lopes, a developmental biologist at Leiden University in the Netherlands, where she stood, she shrugged over Zoom. “I’m not sure,” she told me. “Some people might say that [at 15 days] there’s an early, early progenitor of the brain. But a week later, it’s still a progenitor. And a week after that. It’s still not a brain.”
A couple of years ago, scientists representing the International Society for Stem Cell Research (ISSCR) recommended that the 14-day rule be relaxed somewhat. Rather than being completely banned, research on human embryos that goes beyond 14 days should be subject to an ethical and regulatory review, they wrote.
What about blastoids? For a start, it would be difficult to apply the 14-day rule in the same way, says Janet Rossant, a developmental biologist at the Hospital for Sick Children in Toronto and an ISSCR steering committee member. With human embryos, the clock starts ticking from the moment of fertilization, which is when the sperm successfully fertilizes the egg. This doesn’t happen when you make a blastoid from stem cells. So when should you start counting? From when you put the cells in a dish? From the first time the cells divide? Or the second?
Perhaps the bigger question rests on how embryo-like these stem-cell-derived structures are. For some scientists, it’s a catch-22 situation. If the blastoids look too much like embryos, then many believe research with them should be restricted in the same way that we control work on human embryos.
But if they don’t look enough like embryos, then there’s no point in using them for research, says Chuva de Sousa Lopes. “At the moment, it’s so difficult to understand how close they are, or how different they are,” she says.
Scientists tend to look at the size and shape of the structures, and which genes their cells express, to work out how similar they are to typical embryos. But there are other important aspects to consider.
“We first need to agree on what an embryo is,” says Naomi Moris, a developmental biologist at the Crick Institute in London. “Is it the thing that is only generated from the fusion of a sperm and an egg? Is it something to do with the cell types it possesses, or the [shape] of the structure?”
Perhaps it’s more to do with the structure’s potential. A human embryo could go on to form a person. Human blastoids can’t develop into people. Yet.
As the technology advances, it is looking increasingly likely that one day, stem-cell-derived embryos will be able to develop into living animals. “Theoretically, if you have all the right cell types … they could go further,” says Rossant. “Never say never.”
However we define blastoids and other embryo-like structures, now is the time to start regulating how we grow and study them. Rossant is one of the many scientists I spoke to who agree that, given how embryo-like these structures are looking, they should probably be subject to the same rules and regulations that cover research on normal embryos.
“The big risk is … if we had one rogue player that went really fast [with human cells], and developed something that caused a public backlash,” says Moris.
Jianping Fu, a bioengineer at the University of Michigan in Ann Arbor, has similar concerns. “Given how rapidly the field has been moving over the last few years … I’ve become more and more concerned about how close we are to generating a complete human embryo model with the potential to develop into a viable human embryo or fetus,” he says. “This is not some far-fetched, remote possibility.”
Read more from Tech Review’s archive
You can read more about the new study in monkeys, and what happens to the synthetic embryos when they are implanted into animals, here.
My colleague Antonio Regalado has been covering these advances for a while. Back in 2017, he pointed out that “artificial embryos” were coming, and that no one knew what to do with them.
These embryo-like structures were featured as one of Technology Review’s top 10 breakthrough technologies of 2020. Antonio explained why here. (And here’s this year’s list, in case you missed it!)
In the last year, scientists have pushed stem-cell-derived embryos further than ever before. My colleague Rhiannon Williams wrote about mouse embryos created this way, which showed more brain development than had been seen previously.
And Antonio has covered similar work that resulted in mouse embryoids with a beating heart. The researcher behind that work plans to develop human cells in the same way—to eventually grow new organs for transplantation.
From around the web
The first CRISPR treatment for sickle-cell disease has been submitted to the US Food and Drug Administration. Vertex, the company behind the treatment, has requested a priority review from the FDA. If approved, the treatment could become available by the end of the year. (STAT)
Ten years ago, pancreas cells from newborn pigs were transplanted into 14 people with diabetes. A decade later, most of them have better control over their blood sugar levels, and say they would recommend the treatment. (Xenotransplantation)
Lab-grown fat, anyone? Scientists have managed to grow fatty tissues from cells in the lab, and hope to use them to make lab-grown meat more meat-like. (eLife)
Ozempic has been all over the news lately. But a host of other weight-loss drugs are on the horizon. (The Atlantic)
Remember the brouhaha about samples collected from the infamous wet market that has long been considered the epicenter of the covid-19 outbreak? The Chinese scientists who collected the samples have finally published their research. Their paper suggests that humans might have brought the virus to the market, rather than the other way around. But not everyone is convinced by the study—not least because it suggests pandas were at the market, despite the fact that killing a panda carries the death sentence in China. (Nature)