The many uses of mini-organs
This article first appeared in The Checkup, MIT Technology Review’s weekly biotech newsletter. To receive it in your inbox every Thursday, and read articles like this first, sign up here.
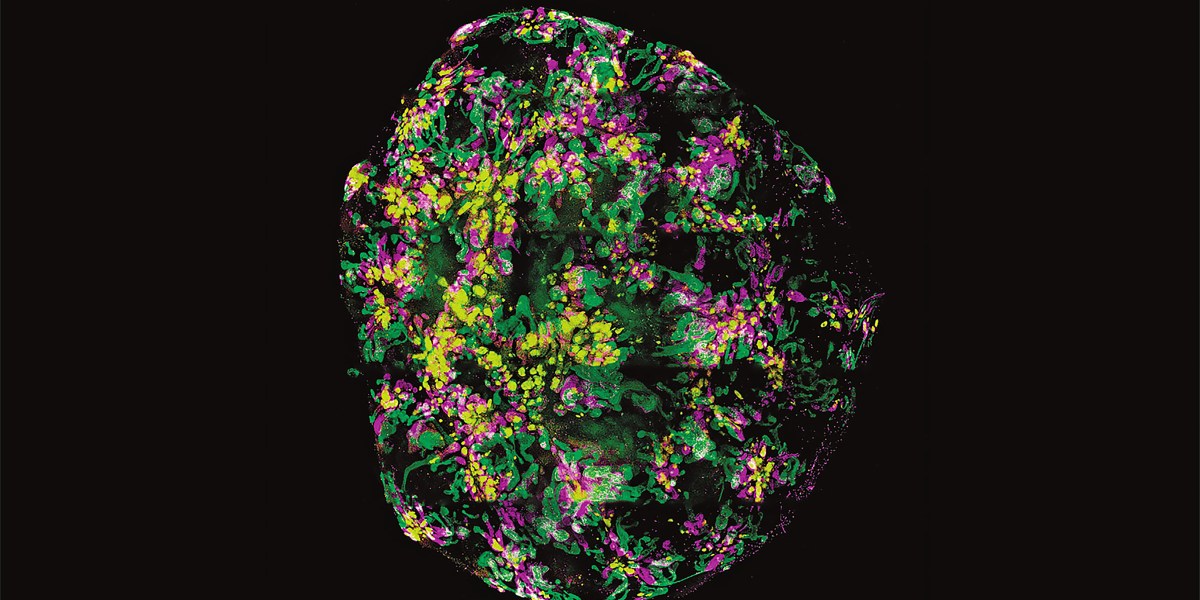
This week I wrote about a team of researchers who managed to grow lung, kidney, and intestinal organoids from fetal cells floating around in the amniotic fluid. Because these tiny 3D cell clusters come from the fetus and mimic some of the features of a real, full-size organ, they can provide a sneak peek at how the fetus is developing. That’s something nearly impossible to do with existing tools.
An ultrasound, for example, might reveal that a fetus’s kidneys are smaller than they should be, but absent a glaring genetic defect, doctors can’t say why they’re small or figure out a fix. But if they can take a small sample of amniotic fluid and grow a kidney organoid, the problem might become evident, and so might a potential solution.
Exciting, right? But organoids can do so much more!
Let’s do a roundup of some of the weird, wild, wonderful, and downright unsettling uses that researchers have come up with for organoids.
Organoids could help speed drug development. By some estimates, 90% of drug candidates fail during human trials. That’s because the preclinical testing happens largely in cells and rodents. Neither is a perfect model. Cells lack complexity. And mice, as we all know, are not humans.
Organoids aren’t humans either, but they come from humans. And they have the advantage of having more complexity than a layer of cells in a dish. That makes them a good model for screening drug candidates. When I wrote about organoids in 2015, one cancer researcher told me that studying cells to understand how an organ functions is like studying a pile of bricks to understand the function of a house. Why not just study the house?
Big Pharma appears to agree. In 2022, Roche hired organoid pioneer Hans Clevers to head its Pharma Research and Early Development division. “My belief is that human organoids will eventually complement everything we are currently doing. I’m convinced, now that I’ve seen how the whole drug development process runs, that one can implement human organoids at every step of the way,” Clevers told Nature.
Organoids are trickier to grow than cell lines, but some companies are working to make the process automated. The Philadelphia-based biotech Vivodyne has developed a robotic system that combines organoids with organ-on-a-chip technology. The system grows 20 kinds of human tissue, each containing 200,000 to 500,000 cells, and then doses them with drugs. These “lab-grown human test subjects” provide “huge amounts of complex human data—larger than you could get from any clinical trial,” said Andrei Georgescu, CEO and cofounder of Vivodyne, in a press release.
According to Viodyne’s website, the proprietary machines can test 10,000 independent human tissues at a time, “yielding vivarium-scale output.” Vivarium-scale output. I had to roll this phrase around my brain quite a few times before I understood what they meant: the robot provides the same amount of data as a building full of lab mice.
Organoids could help doctors make medical decisions for individual patients. These mini organs can be grown from stem cells, but they can also be grown from adult cells that have been nudged into a stem-like state. That makes it possible to grow organoids from anyone for any number of uses. In cancer patients, for instance, these patient-derived organoids could be used to help figure out the best therapy.
Cystic fibrosis is another example. Many cystic fibrosis therapies are approved to treat people with specific mutations. But for people who have rarer mutations, it’s not clear which therapies will work. Enter organoids.
Doctors take rectal biopsies from people with the disease, use the cells to create personalized intestinal organoids, and then apply different drugs. If a given treatment works, the ion channels open, water rushes in, and the organoids visibly swell. The results of this test have been used to guide the off-label use of these medications. In one recent case, the test allowed a woman with cystic fibrosis to access one of these drugs through a compassionate use program.
Organoids are also poised to help researchers better understand how our bodies interact with the microbes that surround (and sometimes infect) us. During the Zika health emergency in 2015, researchers used brain organoids to figure out how the virus causes microcephaly and brain malformations. Researchers have also managed to use organoids to grow norovirus, the pathogen responsible for most stomach flus. Human norovirus doesn’t infect mice, and it has proved especially tricky to culture in cells. That’s probably part of the reason we have no therapies for the illness.
I’ve saved the weirdest and arguably creepiest applications for last. Some researchers are working to leverage the brain’s unparalleled ability to learn by developing brain organoid biocomputers. The current iterations of these biocomputers aren’t doing any high-level thinking. One clump of brain cells in a dish learned to play the video game Pong. Another hybrid biocomputer maybe managed to decode some audio signals from people pronouncing Japanese vowels. The field is still in extremely early stages, and researchers are wary of overhyping the technology. But given where the field wants to go—full-fledged organoid intelligence—it’s not too early to talk about ethical concerns. Could a biocomputer become conscious? Organoids arise from cells taken from an individual. What rights would that person have? Would the biocomputer have rights of its own? And what about rodents that have had brain organoids implanted in them? (Yes, that’s happening too).
Last year, researchers reported that human organoids implanted in rat brains expanded into millions of neurons and managed to wire themselves into the animal’s brain. When they blew a puff of air over the rat’s whiskers, they could record an electrical signal zipping through the human neurons.
In a 2017 Stat story on efforts to implant human brain organoids into rodents, the late Sharon Begley talked to legal scholar and bioethicist Hank Greely of Stanford University. During their conversation, he invoked the literary classic Frankenstein as a cautionary and relevant tale: “it could be that what you’ve built is entitled to some kind of respect,” he told her.
Now read the rest of The Checkup
Read more from MIT Technology Review’s archive
In 2023, scientists reported that brain organoids hitched to an electronic chip could perform some very basic speech recognition tasks. Abdullahi Tsanni has the story.
Saima Sidik tells us how organoids created from the uterine lining might reveal the mysteries of menstruation. Here’s her report.
When will we be able to transplant mini lungs, livers, or thyroids into people? Ten years … maybe, said my colleague Jess Hamzelou in this past issue of The Checkup.
From around the web
An Alabama bill passed on Wednesday creates a “legal moat” around embryos. Under the new law, providers and recipients of IVF could not be prosecuted or sued for damaging or destroying embryos. But the law doesn’t answer the central question raised by Alabama courts last week: Are embryos people? (NYT)
More legal news. The Senate homeland security committee passed a bill this week that would block certain Chinese biotechs from conducting business in the US. The aim is to keep them from accessing Americans personal health data and genetic information. But some critics have raised supply chain concerns. (Reuters)
Some scientists have expressed concern that too many covid shots could fatigue the immune system and make vaccination less effective. But a man who got a whopping 217 covid vaccines showed no signs of a flagging immune response. (Washington Post)
Buckle up. Norovirus is coming for you. (USA Today).Small studies showing that ibogaine, a psychedelic derived from tree bark, can treat opioid addiction have renewed interest in this illegal drug. But some researchers question whether it could ever be a feasible therapy (NYT)